Diabetes and the Feet
- Super User
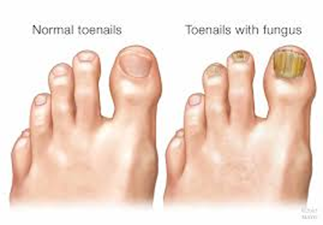
Diabetic Neuropathy
Diabetes is the leading cause of neuropathy in North America. 
Neuropathy is the lack of feeling or sensation.
With diabetes, you tend to lose sensation in your extremities, especially your feet. Damage to the nerves is mainly caused by high blood sugar levels and increased inflammation.
Neuropathy is the leading cause for disability: it increases your risk for foot ulcers, amputations and/or fall related injuries.
Foot Deformities
With diabetes, the nerves affecting your feet and leg muscles do not work properly causing weakness. This leads to a condition called the intrinsic minus foot.
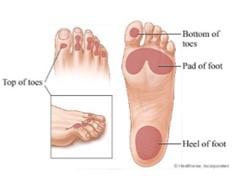
The following are characteristics of an intrinsic minus foot:
- An increasingly high arch
- Digital deformities such as hammer toes and claw toes
- Prominent pressure points under the ball of your feet
These foot deformities put you at risk of ulceration.
This is why it is important to have appropriate size footwear!

Diabetic Foot Ulcers
Diabetic foot ulcers can consist of small cuts, scrapes or blisters that can develop into larger wounds.
Having diabetes tends to slow down wound healing.
Feet are most commonly affected. If left untreated, these ulcers can become a serious health issue and can possibly lead to an amputation.
It is very important to monitor your feet daily and catch wounds early!
Call 613-435-3020 if you have any questions!
|
THE DOS AND DON’TS OF DIABETIC FOOT CARE |
|
|
DO… |
DON’T… |
|
- Wear well-fitted shoes (check inside your shoes before putting them on to make sure there are no rocks/objects)
- Wear socks (make sure they are seamless, white socks help visualize blood/discharge)
- Wash, inspect and moisturize your feet daily (a mirror helps to see the bottom of your feet, keep in between the toes dry)
- Cover any breaks in the skin with an antiseptic and sterile bandage (polysporin or betadine and a bandaid big enough to cover the lesion)
- Cut your nails straight across (do not cut into the corners)
- Contact a chiropodist if you have any problems with your feet |
- Apply a heat pad directly to your feet
- Pick at any calluses or corns on your feet
- Walk bare feet!!!
- Apply strong chemicals to your feet
- Wear constrictive socks or footwear
- Wear open toe shoes, high heels or worn out shoes
- Get a pedicure by non healthcare professionals
- Smoke (it causes poor circulation to your feet)
|